This report describes the outputs and outcomes from the NHS: Best Place to Work tweet chat that took place between 7pm and 8pm on 9 September 2019.
A tweet chat is a scheduled, organised conversation on Twitter focused around a specific topic. Anyone can join in a tweet chat, using the designated tweet chat hashtag, in this case #OurNHSPeople.
This report is written in the spirit of the tweet chat. So, for instance, we have included hyperlinks to the Twitter accounts of all the people we mention in the report. Click on the hyperlink (the blue text) to go to the Twitter account of the person named or to the tweet they sent.
The tweet chat was led by Prerana Issar (NHS Chief People Officer) , Navina Evans (Chief Executive of the East London Foundation Trust, and Chair of the Best Place to Work workstream), and Andrew Foster, Chief Executive of Wrightlington, Wigan and Leigh NHS Foundation Trust and lead for the Transforming Leadership Culture workstream). It was facilitated by the NHS Horizons team (@HorizonsNHS) which also prepared this report. The tweet chat lasted for one hour, although the conversation continued actively on Twitter for several days afterwards.
These were the questions asked during the chat:

What happened during the tweet chat?
The core statistics for the tweet chat are as follows:
1872 individuals took part in the tweetchat. They sent 5,228 tweets as part of the tweet chat. The reach of the tweet chat was 4,111,264. This is a count of the unique Twitter accounts that received a tweet about #OurNHSPeople. It represents the size of the audience for our tweet chat conversation. (sources of statistics: Symplur healthcare hashtags and Tweet Binder analytics).
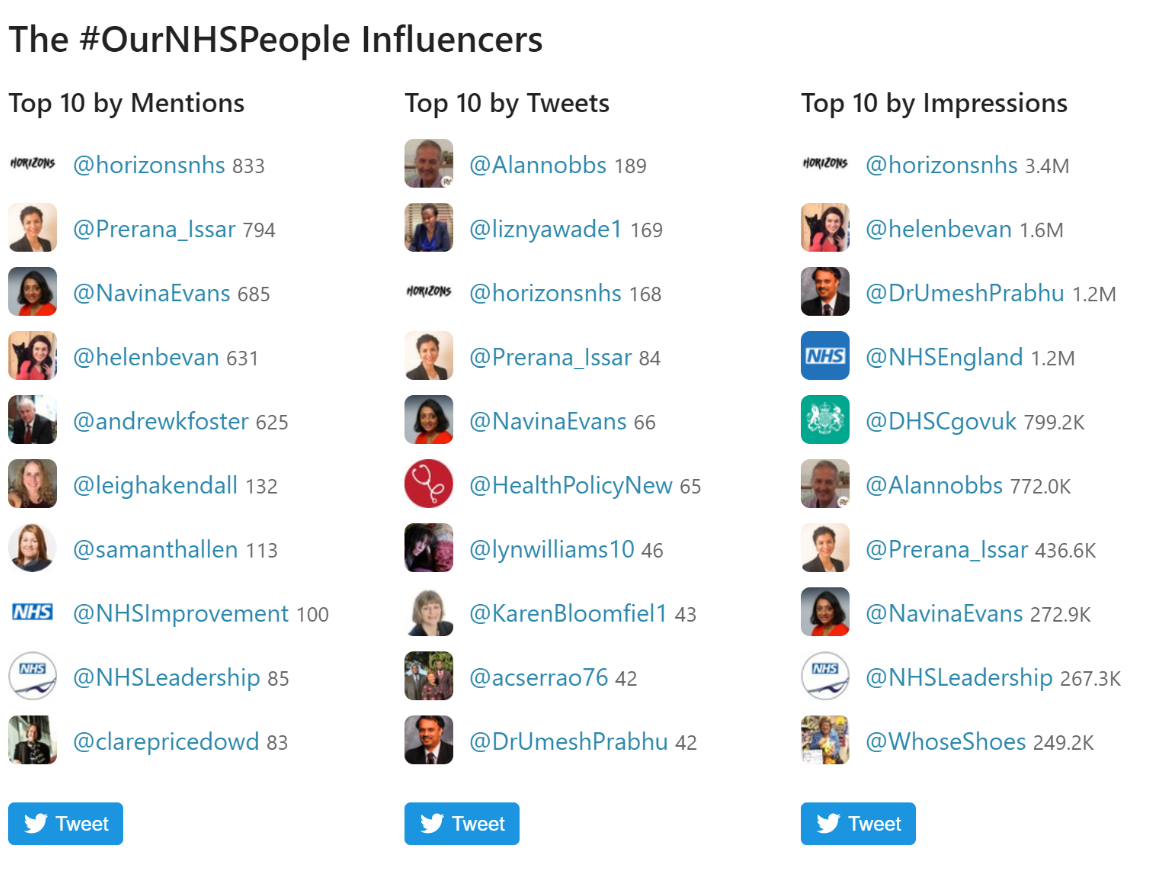
The picture below shows the leading influencers from the tweet chat. The column on the left – “top 10 by mentions” – is of interest, because these are the individuals and organisations that were mentioned by other people most often in their tweets. The second column – “top 10 by tweets” shows who took part in the tweet chat most actively. This shows a wide range of people from across the NHS.
Themes
The Horizons team needed to identify a framework against which to analyse the themes from the tweet chat. There are hundreds of potential leadership models. Our starting point was a traditional leadership framework, such as the McKinsey 7s. It suggests three “hard” S’s (structure, strategy, systems) and four “soft” S’s (shared values, style, skills and staff).

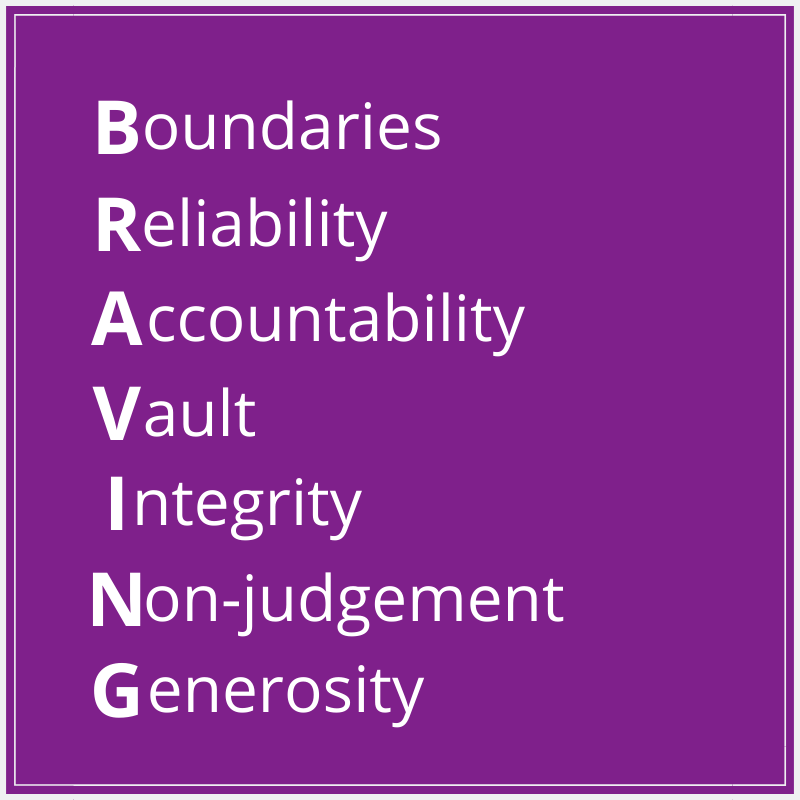
When the Horizons team analysed the tweets, more than 90% of them were about what McKinsey would call soft S’s, so a more nuanced framework was required. After reviewing several models to synthesise that data, we concluded that the best match was Brene Brown’s BRAVING leadership model:
Below is a summary of the contributions to the tweetchat, against the seven headings of the BRAVING model:

We gave each component a letter to make the theming of the tweetchat contributions easier to follow:
- Boundaries.
- Reliability:
- Accountability
- Vault
- Integrity
- Non-judgement
- Generosity
The tweet chat
The first question of the tweet chat asked participants to introduce themselves.
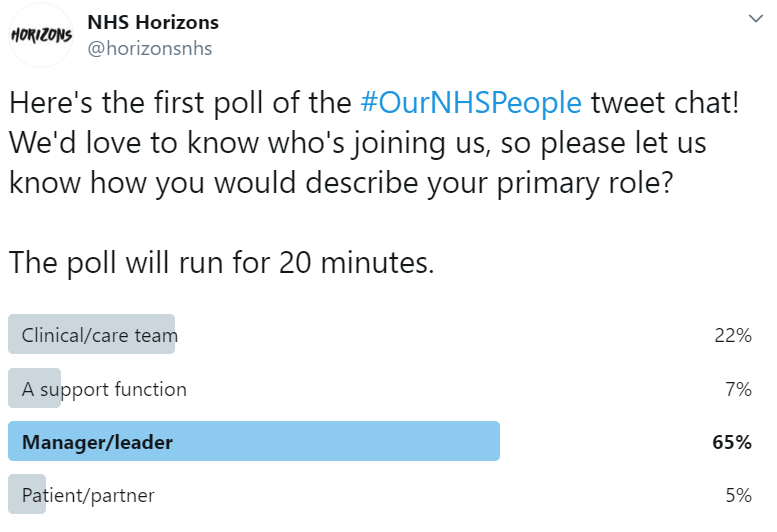
The first poll, asking people to state how they would describe their primary role, ran concurrently. The results are below:
Results from poll 1:
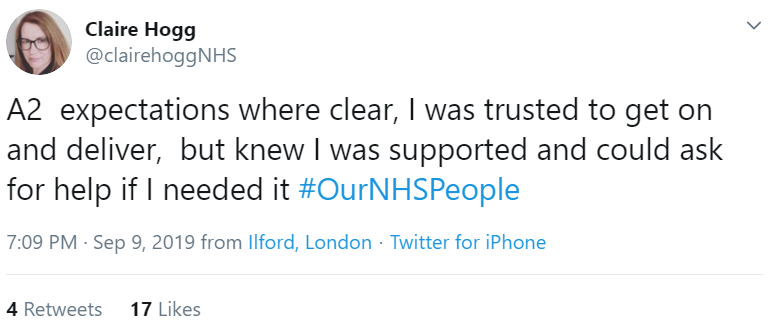
Question 2 (A2): Share an example of when you were well-led. How did it feel?
2.A Boundaries
Flexibility was a much cited topic, as it was in the previous two #OurNHSPeople tweet chats.

Jo Hockley talked about how her need for flexibility and part time working hours was respected – and she returned the favour, for example changing working days when needed. Caroline Poole expressed gratitude at being able to balance work and life without guilt.
Leading by example in setting boundaries helps enable flexible working:


2.B Reliability
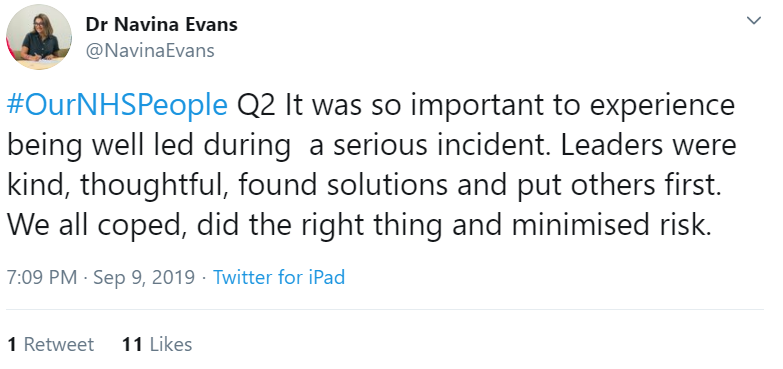
When working in health and care it is likely that at some point staff will be involved in a major incident. Being well-led during such incidents is crucial, as Navina Evans described:
The NHS is a complex system; it is crucial that its leaders are able to communicate effectively:
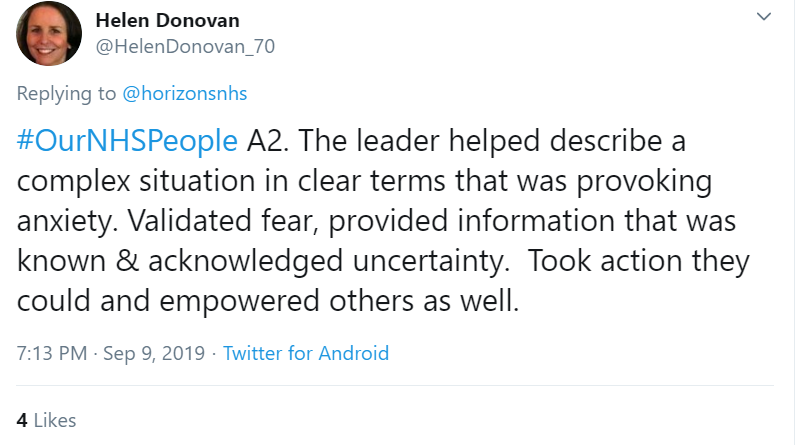
Harriet Brown gave an example of when a leader communicated effectively in challenging circumstances.
Change processes will be familiar to most NHS people. Going through a change process is challenging for everyone – Paul O’Neill shared an example of when his leader took the time to ask about his wellbeing.
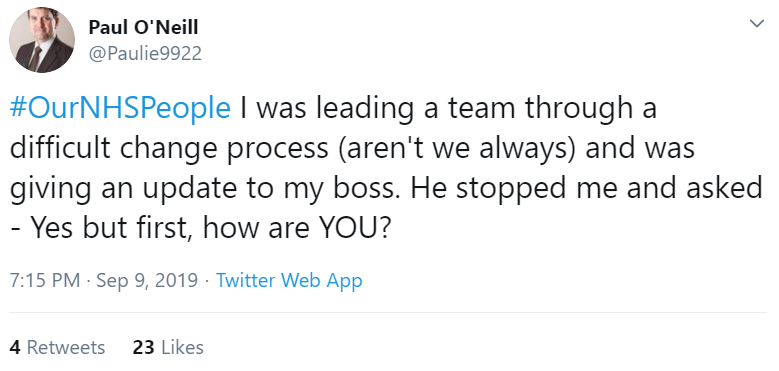
Setting clear expectations had also come up as a topic during the previous tweetchat. Claire Hogg shared an experience where she was trusted to deliver, and knew she was supported.
Samantha Allen had a similar reflection; Becky Carter also talked about role clarity.
Nurse Ali shared a similar experience of feeling encouraged and valued by a manager who is approachable when needed. Being valued and included might sound basic, but it’s so important said Jo Horne. Rachel Pilling said she felt well led be left to get on with a task but have clear understanding of what we are trying to achieve, get regular feedback and access to someone to check on progress and recognition of effort. Dr Ged said he felt his leader supported him to get back in control of issues.
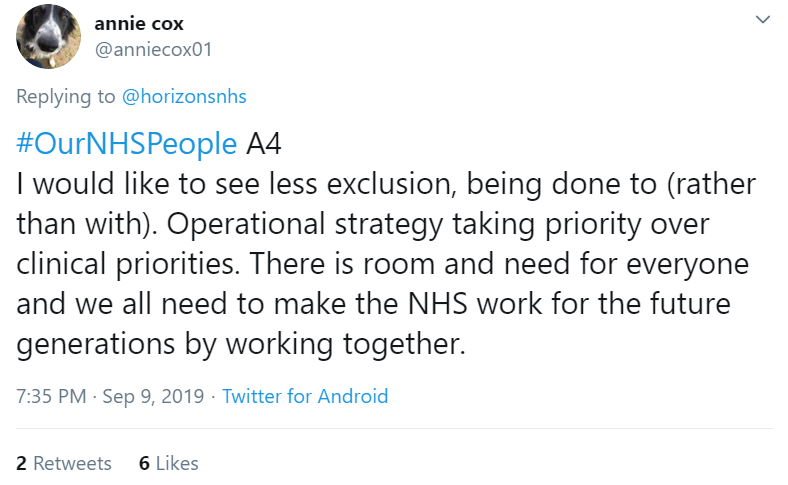
Ann appreciates that her manager values her and her colleagues as people. On a similar theme, Annie Cox said working together is always beneficial – it’s about doing with, not to.
Alan Nobbs shared his experience of being valued, while being given positive challenge.
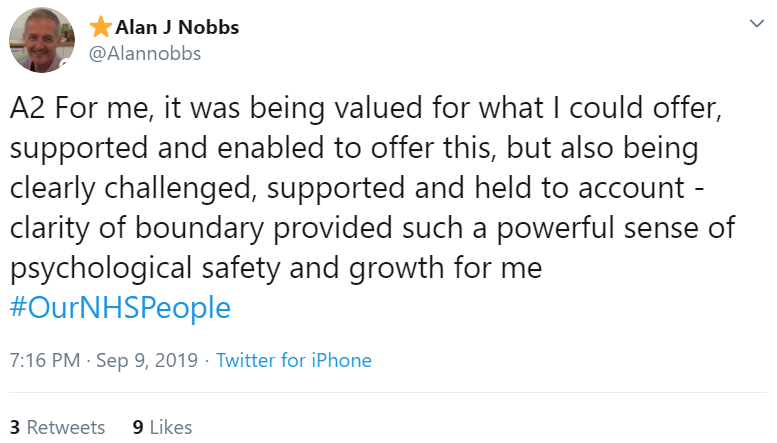
Being well-led makes you feel safe, agreed Claire Price-Dowd; it’s pushing you to be your best, and providing support when needed. Prerana Issar added that in being supported and challenged she could do her best, she could bring her whole self to work…and it was fun! Elizabeth Nyawade said she felt liberated when encouraged to be herself. Jill Page said the leader getting to know people properly meant she felt valued, heard, and worked hard. Helen Bevan said the best leaders make you feel special and loved and help everyone in the team to value their differences.
‘Bandism’ was a returning issue from the previous #OurNHSPeople tweet chat. It is heartening to read Wendy Joberns’ experience of being valued as an equal in a band 2 administrative support role:

Catherine Pelley also talked about being valued irrespective of position in the hierarchy. Laura said everyone being treated as equal was very motivating.
Leading by example by getting stuck in was shared by Ali Aslam:

2.C Accountability
Candour and humility are crucial qualities for a leader. Jo Reynard shared an example:
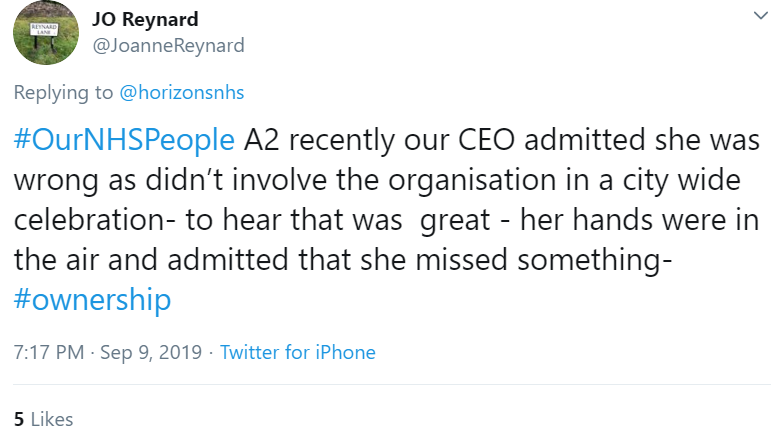
Julie Roberts said she was told early on as a leader to expect to get things wrong, and to make time to reflect on the learning.
2.E Integrity
An effective leader will stand up for their team:


Jill Beech shared a similar experience.
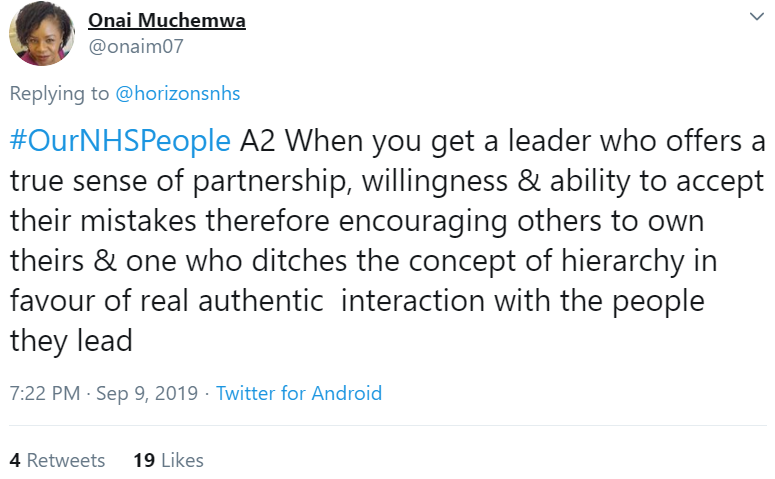
Leaders are human, too: showing vulnerability is important.
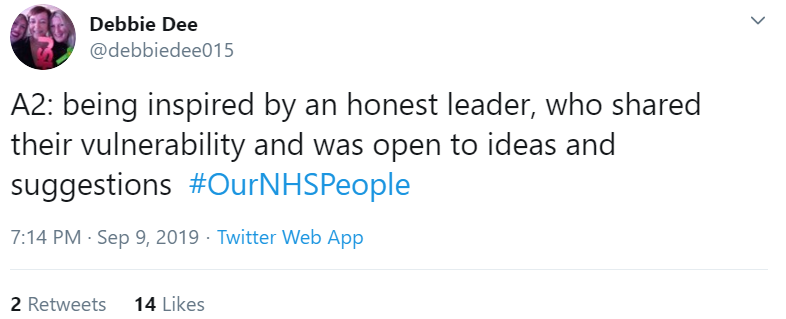
They also have the ability to accept they are not perfect, and are authentic.
Claire Hogg also asked leaders to show vulnerability – and to learn from failures.
An effective leader shows integrity by living their values.


Laura Schaffer said when she felt well-led, there was a clear common purpose that was evident and shared.
Chris Witham described how his leader helped the rest of the organisation understand the function of his team, which helped his team feel valued.
2.F Non judgement
Jo shared that the site director team at North Manchester Care Organisation has a drop-in surgery every two months and she said how important it is to know that the exec team listens.

A supportive working environment was created by a head of department who listened to and acted upon concerns, said Hugh Wilkins. Emma Saunders had a similar experience, adding she felt heard. It’s not always possible to implement ideas: Adrian spoke about the importance of receiving feedback from all ideas.
Stephanie Shillingford described effective leadership where a line manager discussed needed improvements, then encouraged the team to make decisions about what to do together, without them monitoring that discussion, then having the team report back. Cathi felt inspired and motivated on account of being listened to.
Again, being treated equally is important, as with Nathan Sinclair’s experience:

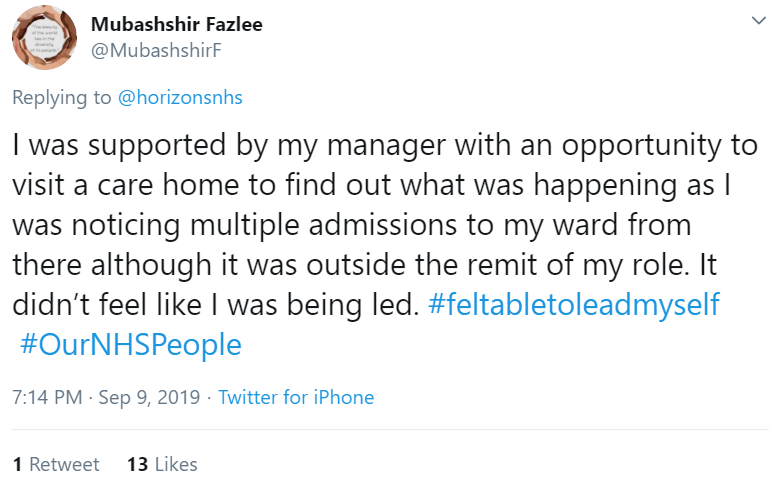
Mubashshir Fazlee was supported to take the right action to support patients.

Knighton Star also said the leader gave permission to make decisions.
Being well-led means people being comfortable enough to challenge upwards, considered Clare Price-Dowd.

2.G Generosity:
Psychological safety is key here.

Amanda Woolley described how a leader encouraged her to try new things, unblocking barriers and remained accountable for the outcome because they were engaged with the people and the process.
Melanie Rowland had a similar experience: she said her leader made her feel like anything was possible, and ensured decision makers were aware she and her fellow Allied Health Practitioners had the answers to issues. Tracy Mellor described being allowed to try out actions without fear of blame if things went wrong.
The second poll of the chat asked people to say how they would describe their immediate line manager. The results are below:

Question 3: (A3) What three qualities do you most need your leader to have?
The responses to this question were collated and compiled in this graphic. The larger a particular word is, the more times it was mentioned in tweets posted by participants.

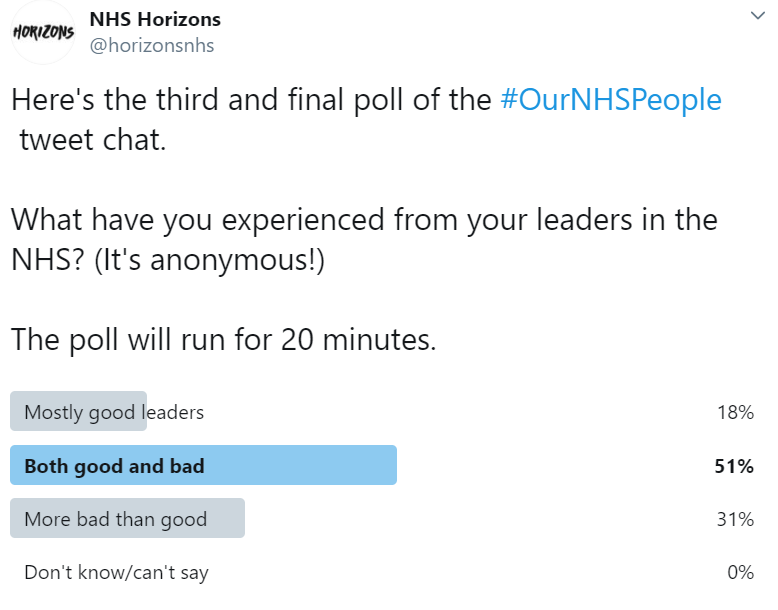
The third poll of the tweet chat asked participants: what have you experienced from your leaders in the NHS? The results are below.
Question 4 and Question 5: (A4 & A5)
What would you like your leader to do more of, and less of? The tweets relating to these questions have been combined below because many of the responses were conflated.
4&5A. Boundaries:
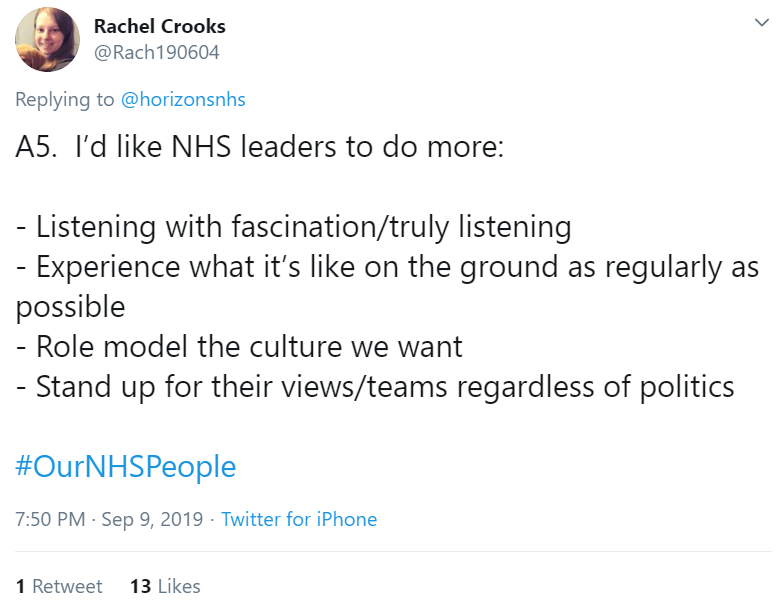
Rachel Crooks asked that leaders lead by example:

There needs to be less of a culture of working ridiculously long hours, and those who don’t being seen as less committed mused Stephanie Thomas. Weir agreed that leaders need to role model positive wellbeing behaviours. Nate considered the toll working pressures can have on wellbeing. Continuing the theme, Michael Butler thought happy staff make happy patients.
Prerana Issar reflected we must be kinder to everyone, including ourselves. We must avoid burnout and remember that kindness is not a weakness said Lynne Bowers. Jacky Francis reminded leaders not to be afraid to show emotion.
Laura Schaffer offered a useful insight about kindness enabling difficult decisions:

Returning to the topic of flexible working, Joanne Hockley asked that it be extended so that part-time workers can aspire to more senior roles.
4&5B. Reliability:
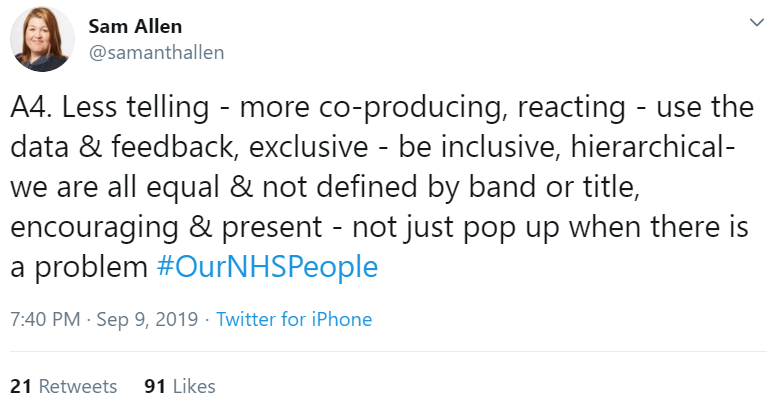
Sam Allen raised the point that NHS leaders need to have core competencies in management and people management skills.

As has been reflected elsewhere, there is no shame in not knowing things, observed Linda Calne – the opportunity to find out leads to amazing outcomes. Ros Penny added that leaders need to admit when they don’t know the answer.
Reducing the time spent in meetings was a popular topic: Prerana Issar felt this is a key leadership skill.

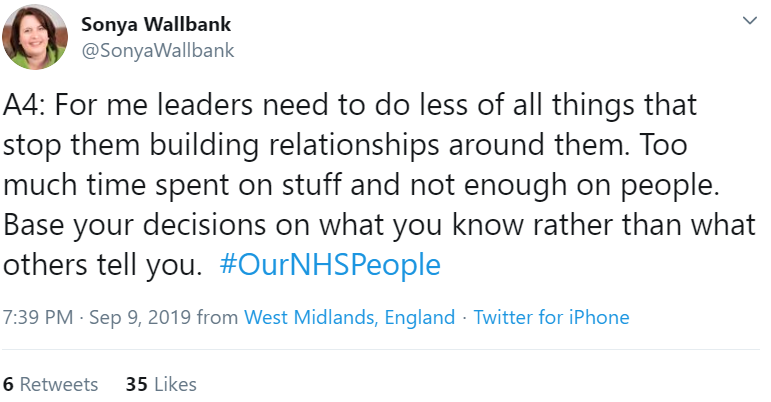
Sonya Wallbank called for less time in meetings, and more time on building relationships.
Poor meeting culture must be challenged, said Jo Horne and Nikki Greenall.
Being in back-to-back meetings can be seen as a ‘badge of honour’ observed Kirstin Gregson. Related to meeting frustration is email frustration: LJ Mottram asked for fewer emails and ‘email ping pong’.
Lyn Williams added acronyms and jargon to frustration with meetings

Gill Phillips had a similar observation.
Rachel Andrew suggested in addition to really getting to know people, leaders encourage ‘reverse gossip’, which is spreading positive feedback.

4&5C. Accountability
Steph Edusei summed up the importance of candour and humility in two outstanding tweets:


Karen also reflected on the importance of honesty. She added thoughts on joy at work.

Honesty about the challenges inherent in leadership could help counter the insecurity talked about by Prerana Issar. She said insecurity leads to micromanagement, and lack of trust with the team.
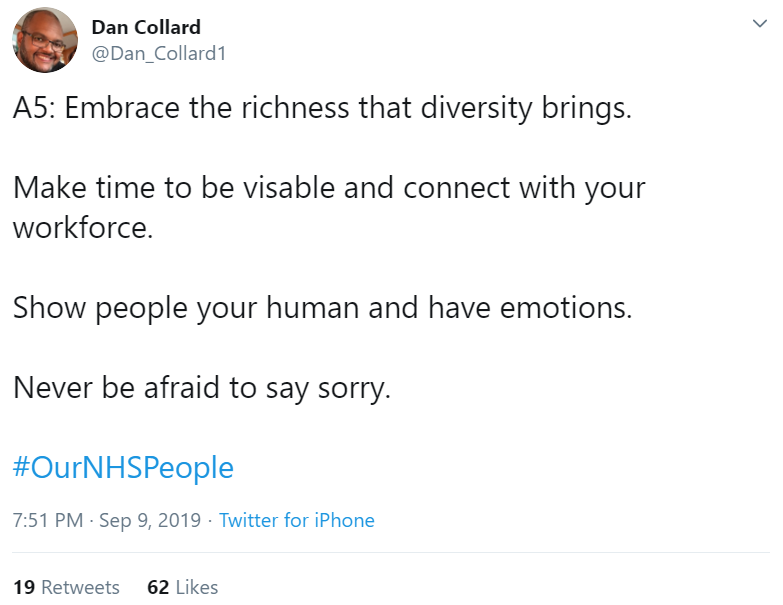
Dan Collard asked that leaders never be afraid to say sorry.
Gaynor Walker offered a similar viewpoint, adding that Agenda for Change is a pay band, not an ability status.

When mistakes are made, learn how to do it differently next time observed Chezzy .
Hugh Wilkins asked for a programme to support whistleblowers. He also identified the creation of unnecessary conflict, and failure to defuse employment disputes created by poor management/leadership as issues affecting people in the NHS.


4&5E. Integrity
Elizabeth Nyawade asked that leaders focus on what is right for patients and staff.


Similarly, Kirstin Gregory asked that leaders offer challenge: are we doing the things that really add value for patient care? She added that effective leadership is willingness to take a stand when it’s the right thing to do, even when it’s unpopular. Fiona Mcnamee reminded leaders to let go of personal agendas – we are all here for our service users and need to pull together. It’s about connecting with our purpose, added Marion Lynch. Pete Gordon said there should be an emphasis on improvement, and to agree a shared purpose that’s focused purely on doing the right things.
Navina Evans asked that leaders spend less time focusing on why things can’t happen; command and control; and ‘management speak’.

‘Management speak’ can be a something to hide behind, commented Susan Griffiths.
Cathi would like to see leaders stop putting themselves before the service.

Paul Sukhu also asked for less focus on internal politics and personal gain. Similarly, Andrew Foster asked for leaders to stop being self-centred, self-important, and selfish.
Andrew also observed that leaders should not manage by fear: you get more out of people in the long term by being nice to them.

Christian Brailsford commented that he would like to see less punative action, risk averse, dishonesty.
High levels of emotional intelligence are needed to enable challenging conversations to occur in a constructive way stated Mike Barnett. He also said leaders need to manage risk, rather than try to eliminate it with draconian control. Leaders need to ‘be comfortable with the uncomfortable’ felt Dr Habib Naqvi .
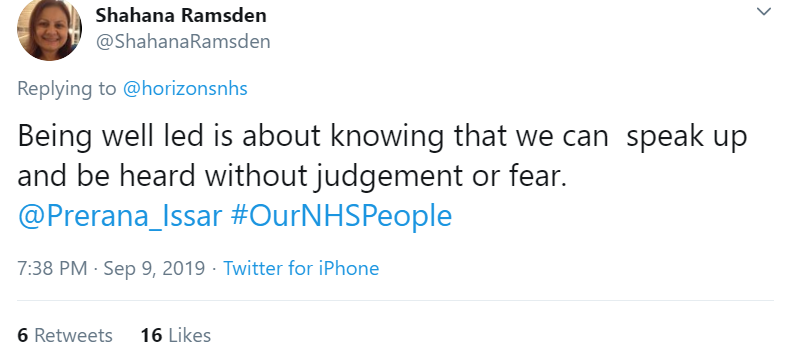
Being well-led is about able to speak up without fear or judgement, felt Shahana Ramsden.
A crucial part of doing the right thing is to challenge bullying.

Bullying was raised as an issue by another Jo, and by Nicola Tyson . Hugh asked for leaders who exhibit bullying behaviour to be held to account. Challenging poor behaviour was raised by Georgie Agass and Jeremy Over. This was echoed by Craig Nikolic, who said too many take the easy option with bullying and discrimination, putting it under the carpet rather than making tough choices.
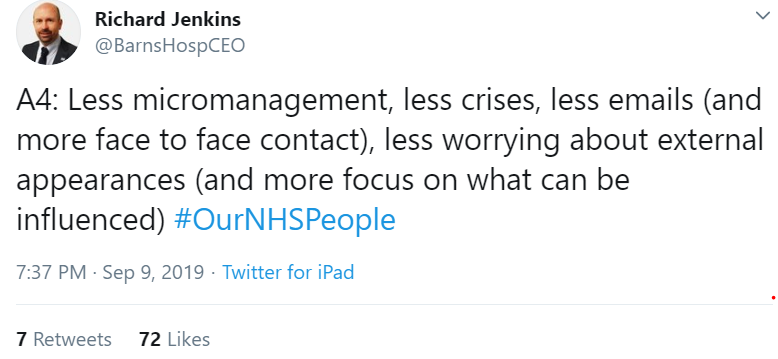
Richard Jenkins asked for leaders to worry less about external experiences, and more about what can be influenced.
Knighton Star said leaders can be disconnected from purpose, spend too much time in offices, achieve the target but miss the point. Annie Cox would also like to see less exclusion, and more working together.
In terms of what leaders should do more of, Alan Nobbs asked for leaders to be more open, more vulnerable, and more courageous.

Nathan Sinclair asked for leaders to accept challenge without defensiveness. Linked to this comment, Paul O’Neill asked for leaders to listen to a wide range of views, not just the most senior or those with whom they already agree:

Kelly Sanghera asked leaders to seek views from those who will be affected by change, as the people who do the job every day will have the best ideas. Annie Cox expanded on this: to be consistent in engaging with staff, and value everyone.

On a similar theme, Jo asked for more listening, to engage with staff they don’t normally meet with, and be honest about what can and can’t be done. Sonya Wallbank added notice the hard work, not just the outputs. Offer development opportunities, asked Harriet Brown.
Ali Aslam asked that leaders make a commitment to inclusion:

The view was echoed by Shahana Ramsden.
4&5F. NO JUDGEMENT
‘No judgement’ is about asking for what you need. Sam Allen’s tweet sums this up succinctly:
Rachel Crook described listening with fascination:
Much better than spending time in meetings, as was a common complaint featured above, is genuinely engaging with staff and listening to what they are saying:
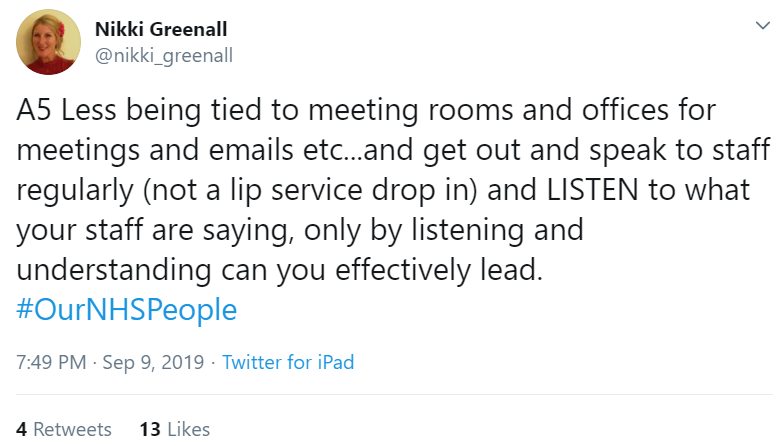
Pete Gordon asked for leaders to spend less time in meetings, more time to go and listen to front line teams. This was echoed by Joanne Mohammed who asked for leaders to spend more time with staff at the front line, really listen to their issues, and act on them; by Debbie Dee; and by Andrea Hargreaves. When people are asked for their views, expectations of what can and can’t be done must be managed, said Jordan Nicholls. Nurse Ali asked for leaders to respond to people; similarly, Jo Horne requested genuine authentic engagement with people, rather than a tick-box exercise, while Stephanie Shillingford said don’t expect people to come to you, go and see them!
Elizabeth Nyawade suggested ‘Gemba Walks’ for meaningful walkabouts.


Charlie Jones wants leaders to understand the complex realities of day-to-day work; he felt a feeling of genuine connection is fostered if leaders understand frustrations and passions.
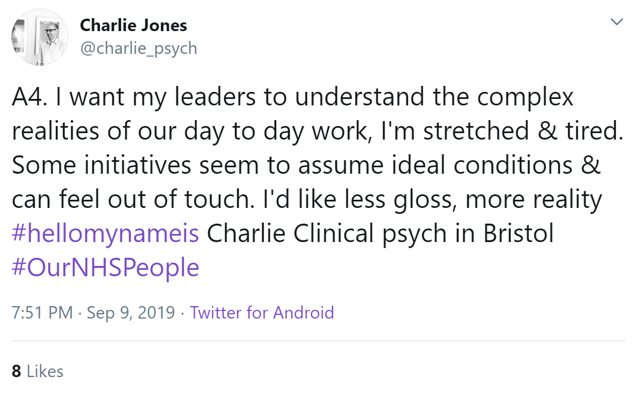
Visibility of leaders was a popular request, as shared for example by Suki Tagger, and by Sue Chisholm who asked for leaders to get ‘in the shoes’ of staff. John Clarke requested that leaders be more than a face on a website, and Steve Palmer said leaders should feel like they have permission to spend more time with their people. Similarly, Helen Bevan asked that leaders spend less time broadcasting, and more time creating spaces (virtual and face-to-face) for people to learn and share; a similar comment was shared by Priyal Shah. Candace Plouffe said leaders need to focus as much as on what’s going well as on areas for improvement.
Emma Saunders asked for leaders to spend more time on the frontline, and shared an example of Board members at the Trust she works at shadowing frontline staff for a full shift:

NHS leaders need to be visible not only to their staff, but to patients too, as shared by Knighton Star, and Debbie Dee who felt leaders should talk to a patient at least once a week.

Cristina Serrao asked for leaders to listen without judgement to patients; it’s more rewarding in the long run. Truly hearing patients and carers was a request from Navina Evans.
The Side by Side Network asked for more coproduction with patients; as Becky Carter observed, we could all be a patient at some time. Emma Challens asked for coproduction to be actively encouraged. ‘Kissing it Better’ suggested stopping in corridors to chat with people – staff and patients. This will help leaders understand the needs of the communities they serve, which was a request by Algar Goredeme-Braid.
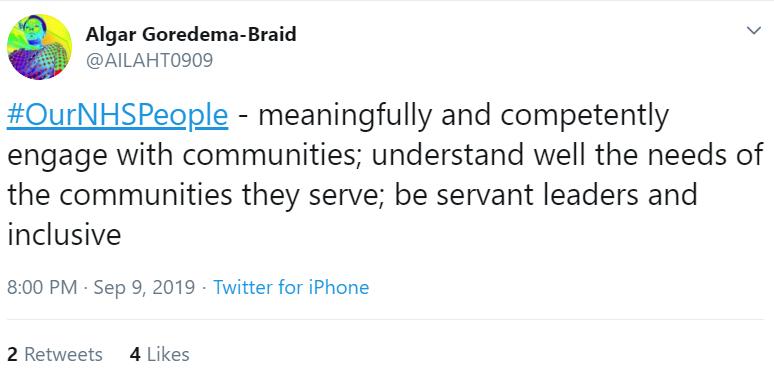
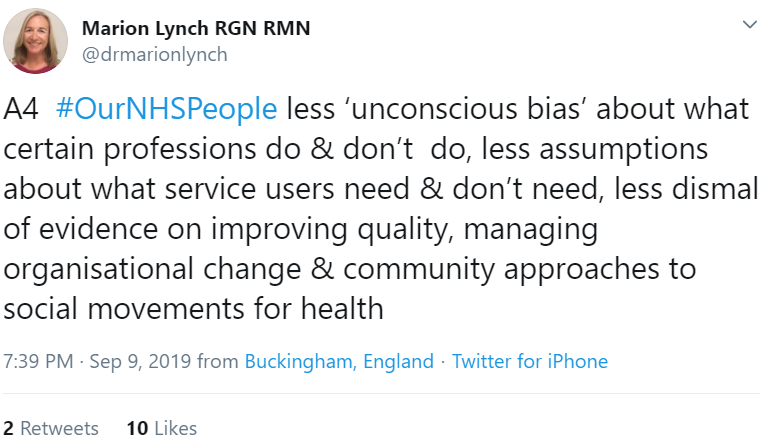
And as Marion Lynch posited, we need to make fewer assumptions about service users do and don’t need, as well as less unconscious bias about what certain professions do and don’t do.
As an elected governor, Jude Goddard asked leaders to get to know governors and non-executive directors to help one another learn and grow.

Mubashshir Fazlee shared a brilliant example of being supported by his manager to do what he saw needed to be done, with positive results for patients:
4&5G. Generosity
Hesham Abdalla asked for people to be treated like adults:

Nurse Ali had a similar reflection; she shared an experience where she had received a ‘telling off’ email from management, where a conversation would have been the better approach.
Stuart Palma suggested the creation of thinking environments, underpinned with psychological safety.

Psychological safety means less ‘meetings and beatings’, as was shared by Laura Schaffer. – and more time to see/hear both reasons and the potential solutions, as well as less blame when failure occurs and the opportunity to share learning.
Psychological safety needs the assumption of positive intent:

Speaking of things that are not easy, empathy is the hardest leadership quality to practise, reflected Kathryn Perera – it is also the most important.


The final poll of the tweet chat asked participants how useful they had found the experience:

Conclusions
Overall, there was a strong sense that people judge their leaders by the quality of their relationships, the extent to which their leaders operate in authentic ways, show compassion and live their values through their actions. This can be seen in the juxtaposition in the response to the polls. When asked about their own line manager, people were generally positive. 40% said their line manger led by example and inspired and 31% said their leader did their best. 29% had a negative view of their own boss. However, when asked about “your leaders from the NHS” more generally, only 18% said they had experienced mostly good leaders and 31% said more they had experienced more bad than good. We conclude that this probably demonstrates the profound relational aspects of leadership. When you have a direct relationship with someone, you are more likely to be positive than if you are observing people in leadership positions more generally.
The tweetchat contributions show us how NHS leaders are signal generators whose words and actions are constantly being scrutinised and interpreted by others, particularly those below them in the organisational structure. So many of the tweetchat comments were about the signals that NHS leaders send about what is important and how to act. It suggests that the actions and behaviours of NHS leaders are amplified far more than the leaders realise and that the signals are far more powerful than leaders think.
This tweetchat demonstrates what a massive responsibility it is to be a NHS leader, not just to deliver excellent care to patients and ensure the performance of the organisation and wider system, but to ensure that everyone in it can bring their best self to work, can thrive and do their best work, every single day.
Leigh Kendall
Helen Bevan
Kathryn Perera
Zarah Mowhabuth
Horizons team



/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-04-14-15-27-52-040-62583d78f636e9115805b2d5.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-08-05-09-59-36-465-62ecea08f636e906acfed639.jpg)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-28-14-57-17-405-62e2a3cdf636e9180c9835cb.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-20-10-16-56-533-62d7d618f636ea07987f6668.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-15-09-55-32-858-62d13994f636ea1398e71aa9.jpg)