This post describes the outputs and outcomes from the NHS: Best Place to Work tweet chat that happened between 7pm and 8pm on 8th July 2019.
A tweet chat is a scheduled, organised conversation on Twitter focused around a specific topic. Anyone can join in a tweet chat, using the designated tweet chat hashtag, in this case #OurNHSPeople.
This report is written in the spirit of the tweet chat. So, for instance, we have included hyperlinks to the Twitter accounts of all the people we mention in the report. Click on the hyperlink (the red text) to go to the Twitter account of the person named or to the tweet they sent.
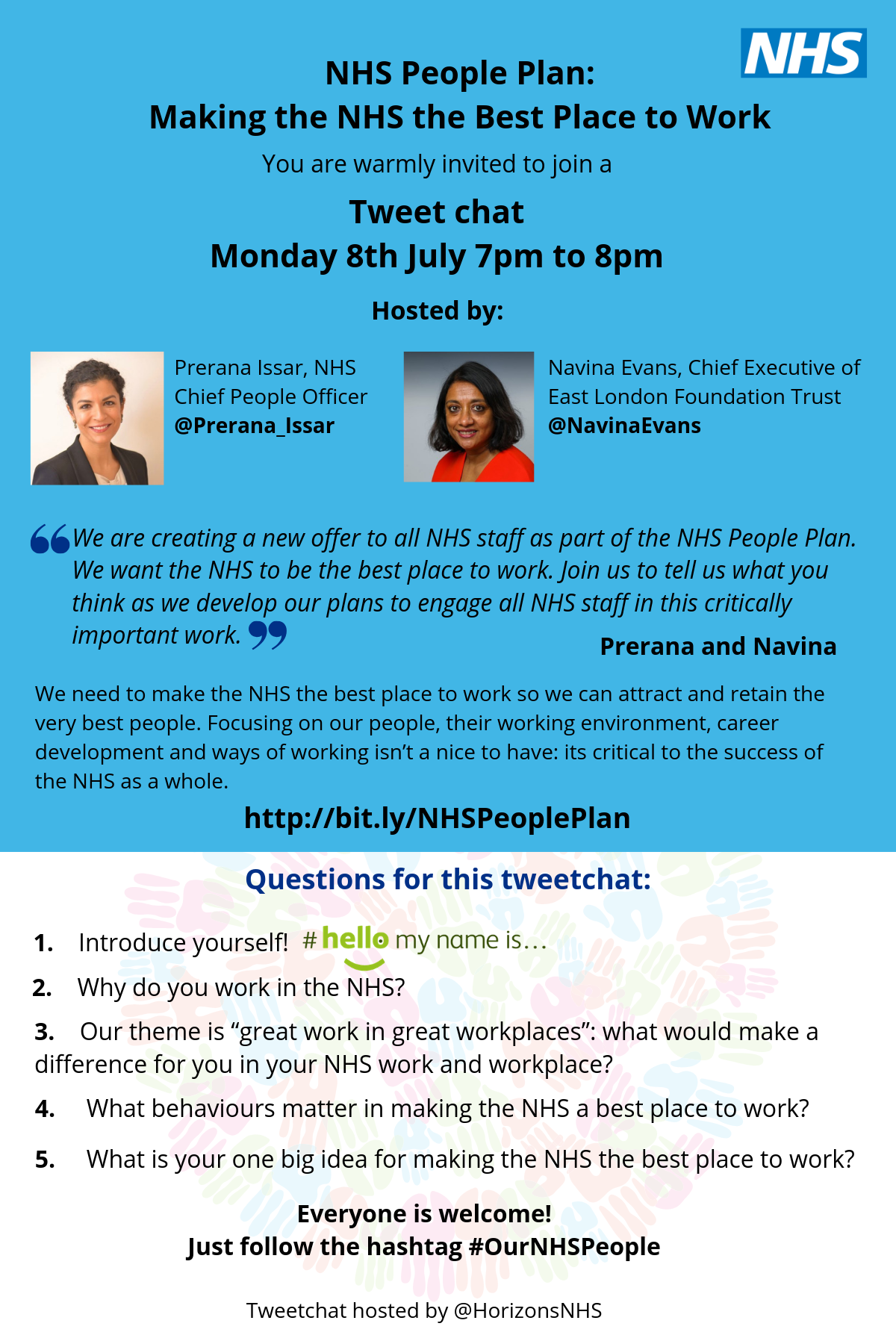
The tweetchat was led by Prerana Issar (NHS Chief People Officer) and Navina Evans (Chief Executive of the East London Foundation Trust, and Chair of the Best Place to Work workstream) It was facilitated by the NHS Horizons team (@HorizonsNHS) who also prepared this report. The tweet chat lasted for one hour, although the conversation continued actively on Twitter for a whole week.
These were the questions asked during the tweet chat:
What happened during the tweet chat?
The core statistics for the tweet chat are as follows:
- By the time that the tweet chat finished at 8pm on 8th July, 1,240 individuals had taken part.
The conversation continued on Twitter:
- By 9am on 9th July, 1,950 people had participated in the Twitter conversation
- By 10am on 10th July, the number of participants was 2,401
- 5,581 tweets were sent as part of the tweet chat
- The reach of the tweet chat was 4,135,409. This is a count of the unique Twitter accounts that received a tweet about #OurNHSPeople. It represents the size of the audience for our tweet chat conversation
This makes the #OurNHSPeople tweet chat probably the biggest, most engaged NHS tweetchat ever (sources of statistics: Symplur healthcare hashtags and Tweet Binder analytics).
The picture below shows the leading influencers from the tweet chat. The column on the left – “top 10 by mentions” – is of interest, because these are the individuals and organisations that were mentioned by other people most often in their tweets. The second column – “top 10 by tweets” shows who took part in the tweet chat most actively. This shows a wide range of people from across the NHS.

The graphic below comes from NodeXL analysis and is a diagrammatic representation of who connected with who during the tweet chat. People on Twitter tend to stick with their own communities and talk virtually to people they know already. These are the clusters we see on the chart. The green lines are where people are communicating and connecting outside of their usual group of people. What is extraordinary about this Twitter conversation is just how many green lines there are. This diagram gives us a strong sense of a large group of people, who wouldn’t normally connect with each other, coming together with shared purpose.

During the tweetchat, our hashtag #OurNHSPeople was the highest trending hashtag in the UK:

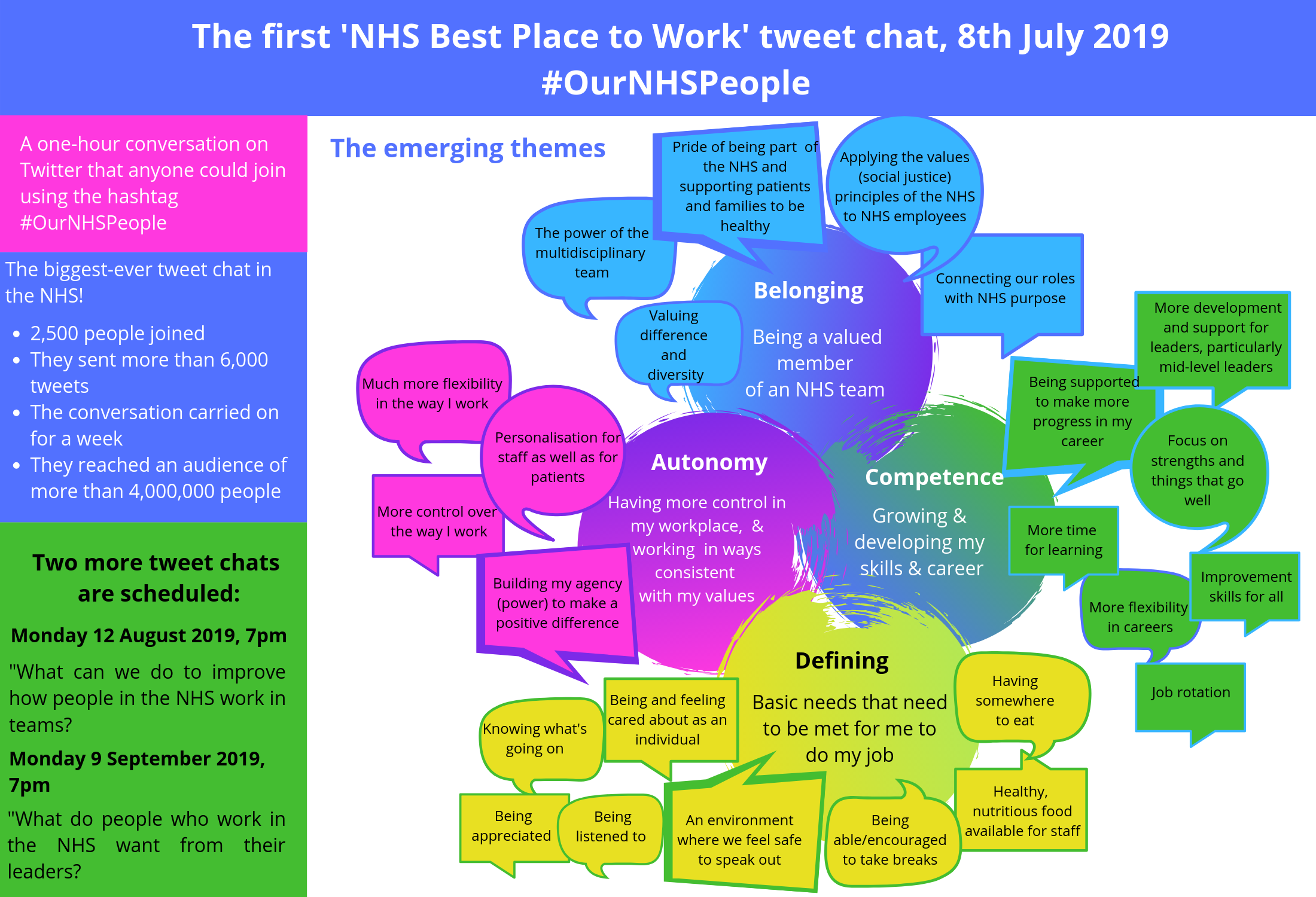
Themes
We analysed the themes from the tweet chat using the model that The NHS Best Place to Work team has adopted for thinking about what will make the NHS the best place to work. The model is called self-determination theory and describes the three core needs people have at work:
- The need for autonomy in the workplace, where people feel they can control their working environment and ensure the work they are doing is consistent with their values and professional integrity;
- The need for belonging, being a valued member of the team or organisation, feeling connection to others and experiencing caring for others;
- The need for competence (this is to do with people growing and developing their skills and feeling like they are doing a good job).
If we fail to meet any one of these needs, it will have a damaging impact on health, wellbeing and motivation at work. If we want the NHS to be the best place to work, we have to create an environment to nurture and meet all three of these needs.
We assessed all the tweets that were posted in the tweet chat against this framework. Overall, there was a good fit. However, we found there were a lot of tweets that needed to be put into an additional category. This was about fundamental or “defining” needs that needed to be met for people to do their jobs properly. This ranged from having food and drink available, being able to take a break or park your car, through to knowing what’s going on and being listened to.
The process of the tweet chat
The first question of the evening asked people to introduce themselves. While moving on to question two, which asked why people work for the NHS, we asked people to answer a poll about how long they had worked in the NHS.
Responses to questions 2, 3, 4, and 5 can be read in the sections below. As far as possible, the responses have been grouped in the themes detailed above. To view the original tweet, click on the hyperlink (the red text).
The results of the poll, which was open for 15 minutes, are below.

65% of the respondents had worked in the NHS for 10 years or more.
Question 2 (A2): Why do you work for the NHS?

Tina Hetherington has worked for the NHS for 25 years; she is continuously inspired by her colleagues who make the impossible happen every day. She referred to how the NHS offers nurses a wealth of opportunities to grow and develop.

This sentiment was echoed by Gayle Hann, who works in the NHS because she believes in free and equal quality healthcare for all. @Anitaobsmed said "Everyone has access at the point of entry. The goodwill and kindness from all the members of staff makes every day at work the best place to be."
Caroline Ogunsola said the NHS brings out the best in her because of the opportunities to make contact with different people and make a positive contribution to their lives. Making a positive impact on people's lives is a motivation shared by Victoria Davies; and Chloe Haigh stated that she believes we must promote health and wellbeing to all.
Andrew Ferguson shared that you get a chance to bring comfort, encouragement, dignity, and a feeling of being listened to every day, for our colleagues as well as our patients.
Paul Jebb wants to make a difference to people, and to ensure the great service continues to improve and be people centred, and by Emma Challens wants to make a difference for people now, and for the future of services. Making a difference is also a motivation for Rachel Crooks.
The contribution from Charlotte Jakab-Hall summed up the sentiments of many others:


This was echoed by Karen Dumain.
The NHS aligning with her values was also a motivation for Bo Escritt; Jane Padmore said she works in the NHS "because it puts people first, the values, the people, the philosophy."

Like many people, Maeve Murray works for the NHS because it has helped save members of her family. Maeve is also passionate about helping all staff grow and develop to their full potential and providing an excellent service to patients and their families. Similarly, Parmjit Kang's life was saved by the NHS, and she now uses her clinical knowledge to help others.



A similar sentiment was shared by Liz Sargeant who also believes in the NHS, but believes that performance culture drives unpleasant behaviours.
Question 3 (A3): Our theme is "great work in great workplaces": what would make a difference for you in your NHS work and workplace?
A3: Autonomy
A big theme was about the need for flexible working practices:
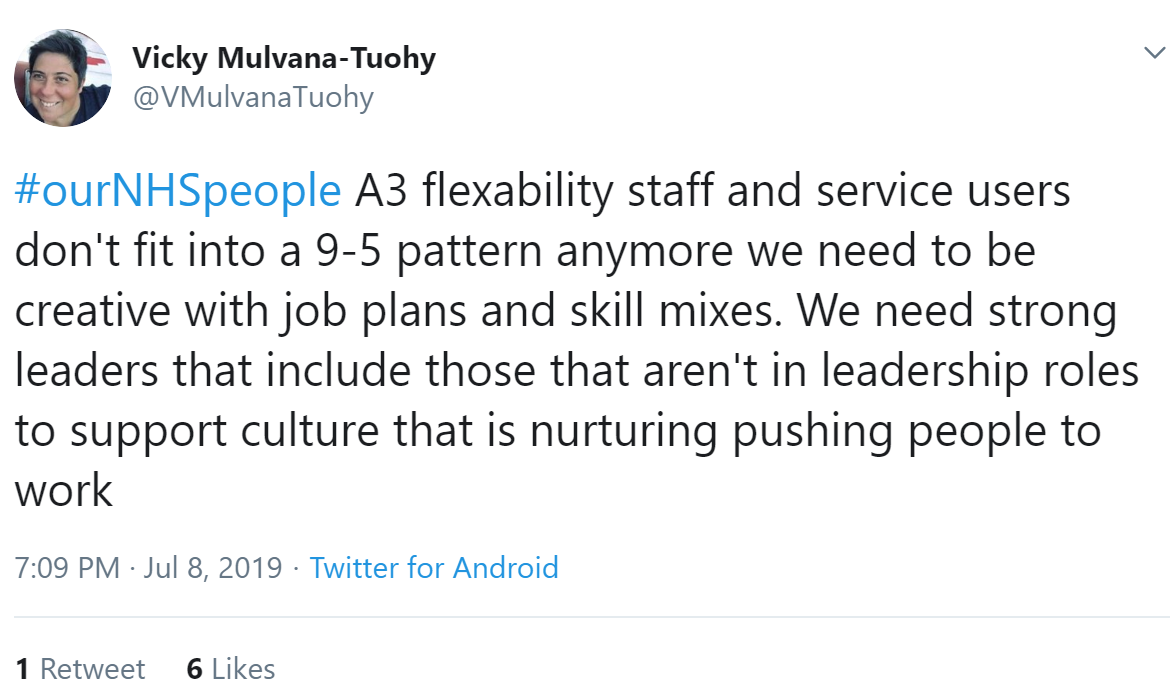
There needs to be more collaborative and empathetic styles of leadership along with more flexibility and engagement for staff, said Daniel Wilder. Flexibility is important to encourage the recruitment of the millennial workforce, observed Jacqui Gladwin.
Chloe Haigh agreed, and said nurses need to be empowered to be leaders.
Hattie Taylor shared an e-bike initiative that is being run at Dorset Health, allowing staff with a choice of how they travel to patient homes, allowing for staff members to feel healthy and stay fit at work, as well as saving time by not having to search for a parking space.
A3: Belonging
Ramblings of a Lady reflected that the support of your team can help you get through a traumatic shift.
Jacqui Gladwin shared her belief that the culture of the NHS needs to reflect the supportive nature and allow staff to grow on their own. In response to Jacqui, Caroline Corrigan added that we need to look after our people so they can look after the patients.
A3: Competence
Robyn Swain questioned whether we should build OD capability in all of our teams and settings to help them reflect and improve? This was exactly the plan of Rachel Andrew's team! Rachel said: "Share the skills, build confidence and competence and help teams/leaders develop themselves and each other."
Knowing that personal & professional development is equally available to all and resources are committed to enable individuals to engage is what Corinna Thomas believed would make a difference in the workplace.
A3: Defining
Nurse Ali agreed that there needs to be better facilities for staff at work.
Pauline Smith added she is concerned about the wellbeing of staff members, and that this may discourage younger people to join the NHS. Jenny Drew shared her experience of having to complete two days of e-learning within her own time before getting a confirmed offer of employment.
In addition, Niall McDermott made the point that the NHS is conglomerate with a lot of variation which means we need to look at what the best teams do to support their staff.
Judith Nembhard added that as NHS employees we should receive better healthcare and made a priority with the interest that staff remain at work.
It is important to treat staff like humans, reflected Andrew Ferguson - this needs to be seen through the wording of HR policies.
Kate Pound said that we need to create an environment where people feel safe: safe in their future, safe to speak up with diversity and safe to feel accepted by all. This was also highlighted by Vijaya Nath who said that we need to name discriminatory behaviour, as once its named it can be tackled.
Katie Macey says she loves her job; the only thing she would change would be to stop 'bandism'; she suggested people ask others' names, rather than their band.
Rachel Crooks agreed and shared that she hadn't heard the word 'stable' used to describe the wider NHS for a very long time. Peter Albert Smith replied that this needed to be change starting from the top; the turnover of CEOs and directors is far too high.
Question 4 (A4): What behaviours matter in making the NHS the best place to work?
A4: Autonomy
In response, Caroline Corrigan said that having voice and control is so important as is development - there are some fab places that really pursue great staff experience.
Andrew Ferguson added that some of this is made worse by not giving those new to management roles enough help and training to deal with the human side of the issues that arise.
Compassion, honesty and getting to know your colleagues were behaviours necessary to Michalis Sanidas: but we also need to learn from things that haven't gone well and avoiding bullying. Rosanna Hunt agreed and replied that we need to facilitate conversations about what is and isn't bullying.
A4: Belonging
Adrian Hayter posited that the behaviours that matter are rooted in the service to others, with active listening, collaboration, openness, honesty, integrity and accountability. This was echoed by Corinna Thomas, who emphasised active listening within teams, departments and organisations with effective, honest and all-encompassing communication.
Fern Berry said it’s important to engage staff from across the board - clinical/nonclinical, Band 1 to the top: "All experiences and opinions matter and feeling like you’re involved in decisions made by the organisation is really rewarding and improves job satisfaction."
Integration and collaboration were key behaviours for Jeanette Renshaw. Suzie Bailey added that a real commitment to collective leadership is necessary.
This was amplified by Jo Meehan who said that staff need to lead by example, setting the tone, and really get to know your colleagues. Leading with respect and authenticity is also an important behavioural trait for Marion Lynch; she added that the space needs to be created for people to flourish and not flounder. If something is not right, we must speak up. @KnightonStar agreed: she said courage is needed in so many areas to effectively challenge poor practice, to advocate for staff and patients and to implement change too.
Camaraderie, shared vision, respect for each other, willingness to learn from each other, thinking positively always are behaviours to be highlighted according to Michael Absoud.

In response, Joanne Mohammed said that the celebration of diversity and inclusive thinking creates inclusive and innovative work places where people are not afraid to voice their ideas of change and improvement.
Diversity comes in many forms: Jonathan Cliffe stated that we must respect individuals for their roles/experience/disciplines can only lead to effective collaboration which can only lead to improved service provision for those we care for.
A4: Competence
 Pete Waddingham added that the behaviour of not being frightened and trying new things is vital.
Pete Waddingham added that the behaviour of not being frightened and trying new things is vital.With the right mindset, leadership skills, passion, motivation and professionalism, things can change for the better said Fernando Francis.
15 seconds 30 minutes said that we need staff to think "How can I thrive today?" rather than "How can I survive today?".
Many behaviours are about being relational: the behaviours that matter to Zoe Moorhouse are honest and transparent conversation where we listen to each other and respect differing opinion, as well as being kind, supportive, and having a little fun! Adding to this viewpoint, David shared that compassionate practise, enabling and alignment to shared goals means recognising the impact of what you do on your team, the system as well as the person you provide care for.
Karen Bloomfield agreed with Kerry, and added the need to encourage, enable and inspire.
Paul Deemer highlighted that the behaviours needed were patience, understanding kindness and clarity, agreed to by Priyal Shah who said there is something about letting people be themselves.
Behaviour breeds behaviour, a culture that nurtures, listens and encourages is always the one that gains the best wins was a reflection shared by Sam Donohue.
Behavioural traits that stand out for Andrew Ferguson are "assuming that people are acting with good intentions...assume the best not the worst. think about the feelings of others. Ask people how they are doing. Look for opportunities to help. Be kind. Do something nice for someone every day. Say hello. Say thanks."
Being compassionate to both staff members and patients was mentioned several times through the tweet chat with points raised by Homerton University Hospital, Jennifer Russell, Anita, Joe Horne, Hannah Morgan and Amanda Oates.
We need to make sure than new NHS staff know that the rest of their working lives are in a good place for them to practice said Amandip Sidhu. Umesh Prabhu responded with the comment that we must care for staff and be kind to staff happy staff means happy patients.
A4: Defining
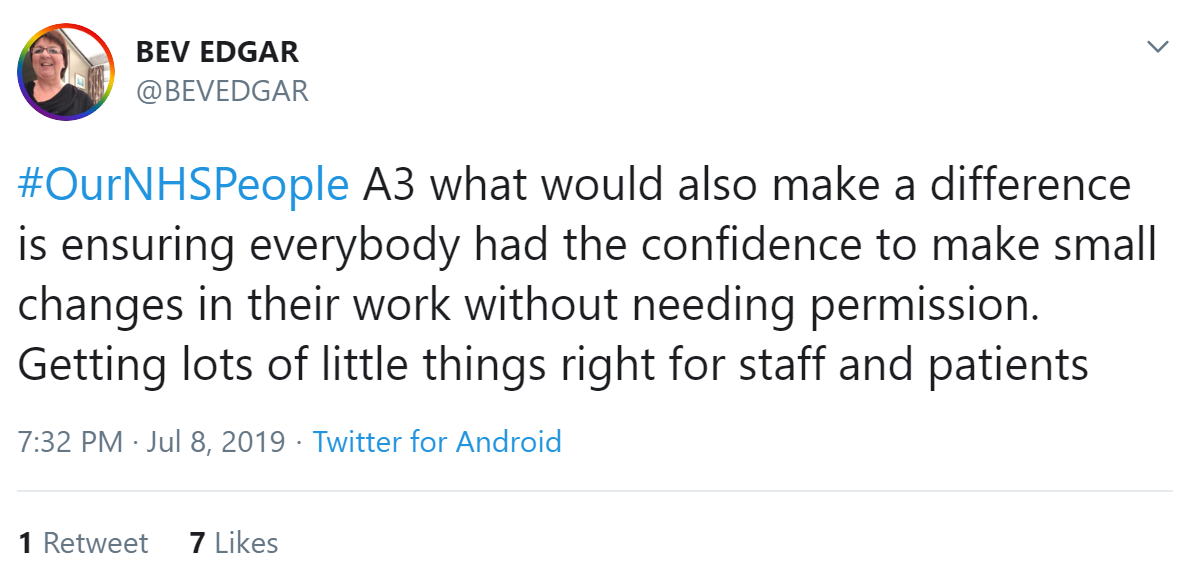
Many of the responses focused on cultures and behaviours that are about getting the small things right that add up to big things. It is about treating staff like human beings with real needs, not widgets.
Question 5: What is your one big idea for making the NHS the best place to work?
A5: Autonomy
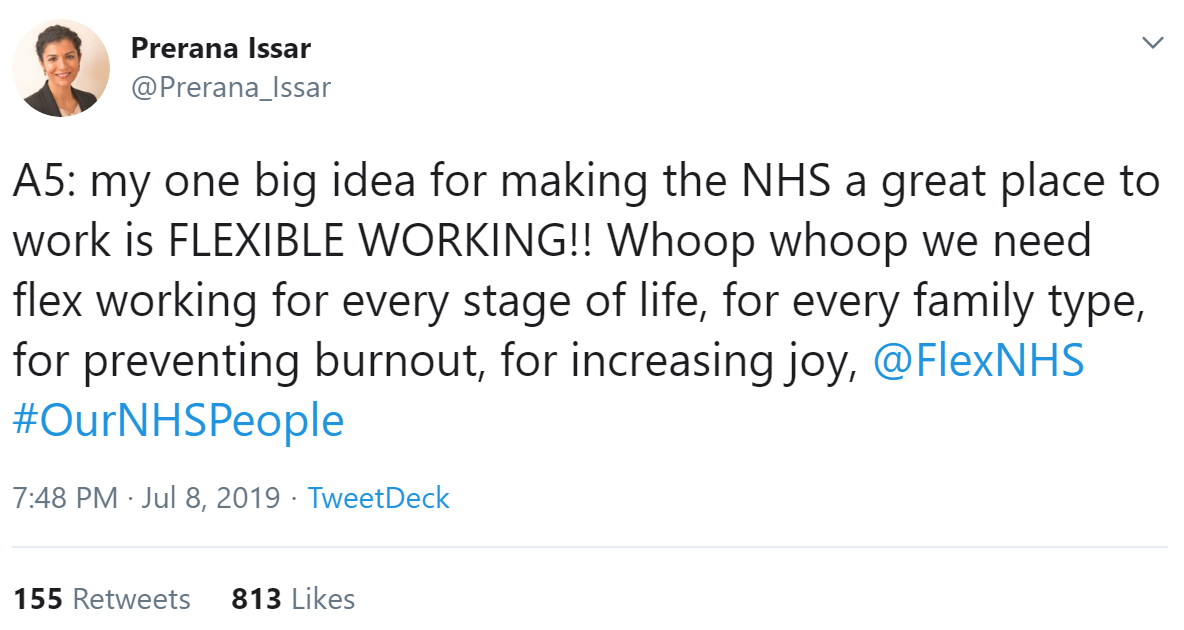
Jane Appleton explained why flexible working is important.
A range of reasons why people might need the opportunity to work flexibly was shared by people including Charlotte Layton, Laura Pisaneschi, Jo Ogidi, Ola Hill, Rachel Crooks, Madiha, Flex NHS, Gaz Davies, Nicole Sahika. As Rachel Waters reflected, flexible working is for everyone; and everyone has different needs, one size doesn't fit all said Paul Sukhu. Personalised care for staff would be a benefit, suggested Helen Bevan. Collette Datt talked about how flexible working worked for her.
 Melissa McGowan encouraged managers to involve everyone, regardless of role or band in decision making. There was another vote for giving staff the time and space to develop their own solutions to problems from Ali Aslam. Vicky's idea was to include everyone in improvement efforts; Ann suggested hierarchies and bureaucracy need to be reduced to enable improvements to happen; and similarly Kerry reflected devolved leadership, honesty and empowerment make for happier teams and therefore better patient outcomes which in turn makes staff happier. This was echoed by Katie Macey, who added staff should be given the freedom to ask forgiveness rather than permission...and going back to joy at work, Laura Schaffer said there should be a sprinkling of fun!
Melissa McGowan encouraged managers to involve everyone, regardless of role or band in decision making. There was another vote for giving staff the time and space to develop their own solutions to problems from Ali Aslam. Vicky's idea was to include everyone in improvement efforts; Ann suggested hierarchies and bureaucracy need to be reduced to enable improvements to happen; and similarly Kerry reflected devolved leadership, honesty and empowerment make for happier teams and therefore better patient outcomes which in turn makes staff happier. This was echoed by Katie Macey, who added staff should be given the freedom to ask forgiveness rather than permission...and going back to joy at work, Laura Schaffer said there should be a sprinkling of fun!All nurses, including primary care, should be on agenda for change suggested Chloe Haigh, while realistic job plans was submitted by Vicky Mulvana-Tuohy.

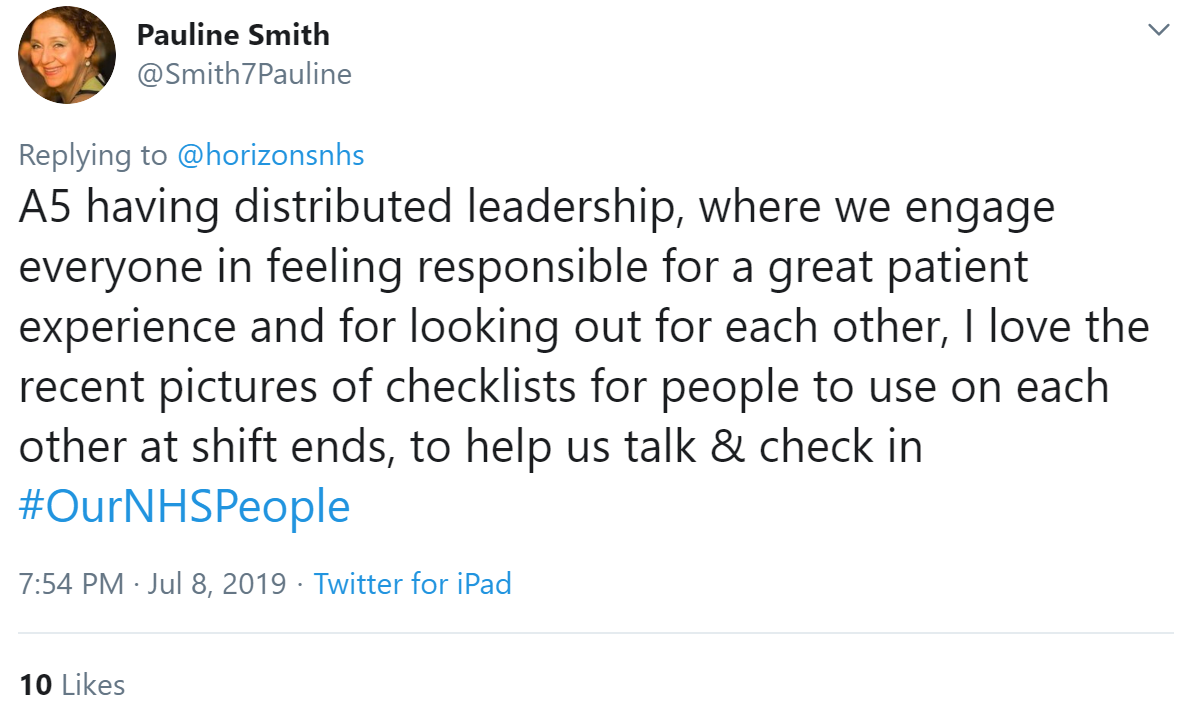
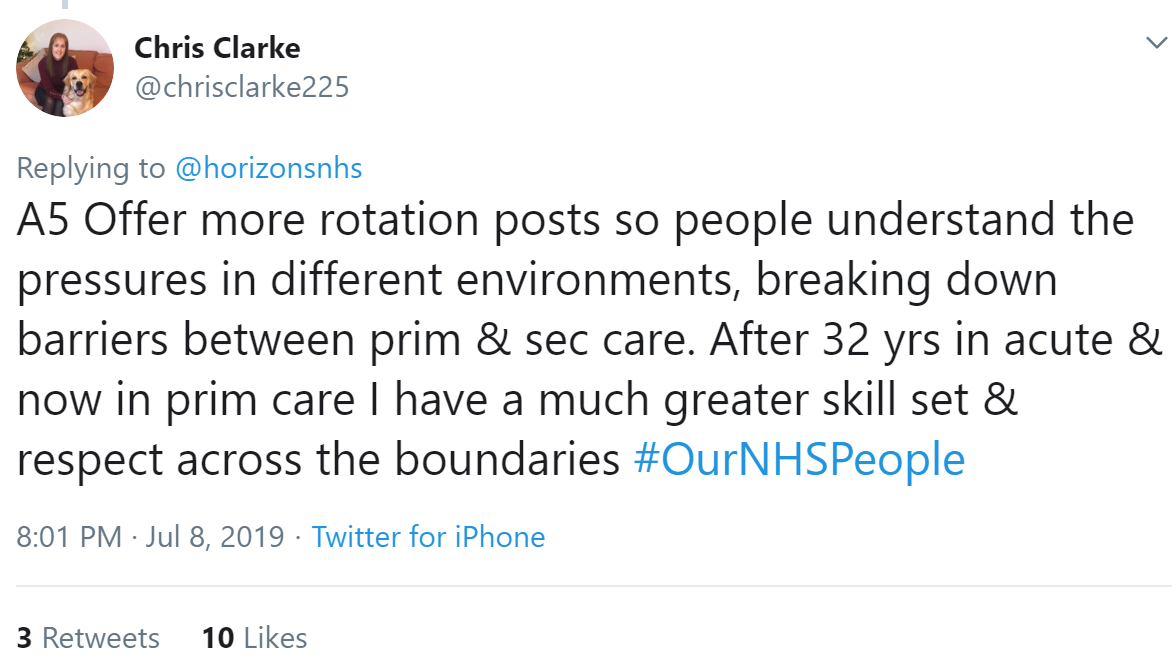
A5: Belonging
A number of ideas centred around shared NHS purpose.
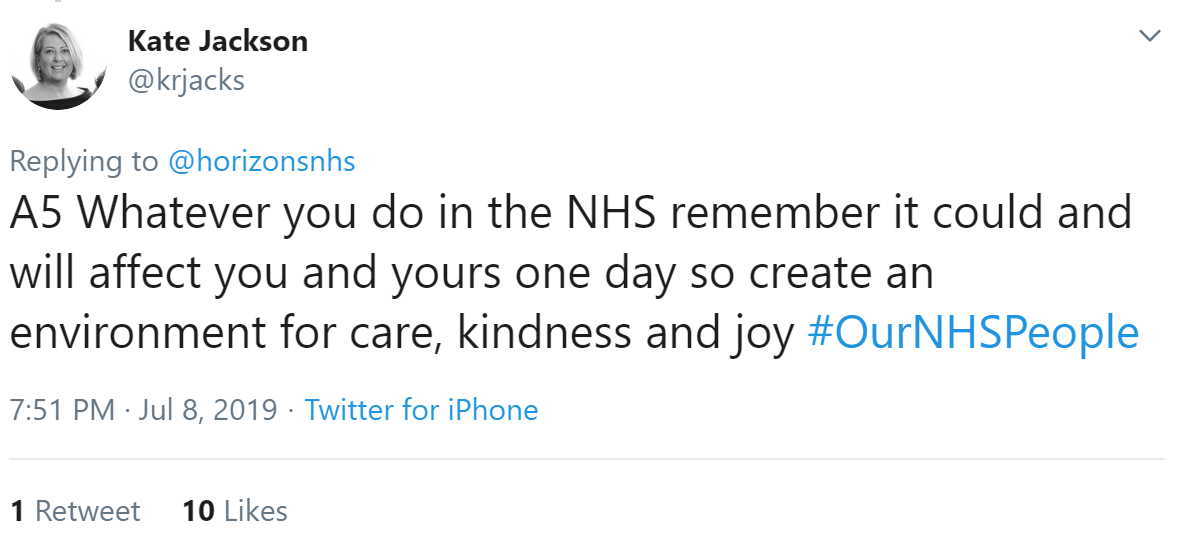
This sentiment was echoed by Helen Conway. The theme was expanded upon by Pete Waddingham: staff can be patients too, so we need to ask colleagues for opinions on improvements.

This could be supported by making staff experience a core objective for boards as was suggested by Katy.
The importance of getting feedback from staff was stated by Raino Bains: "Staff are encouraged to raise their voice to ensure we provide great patient care and experience." Bongi's suggestion echoed this: "A culture of collaboration and an NHS that craves honest feedback from its employees."


Al Richards observed we need to make sure user involvement is more than tokenism.

Treat people fairly, value diversity asked Nazia Ahmed; this was echoed by Hayley Mounsey. "...diversity driving inclusion across all parts of professions, organisations & systems we have to get the mix right to ensure we have challenge to find the answers" was shared by Lisa Hodgson.
Kamilla Kamaruddin said while there has been lots of improvement, she would like to see greater inclusion for trans people.

Continuing this theme, Brian Webster said say thank you, see what has been done rather than focus on what hasn't.
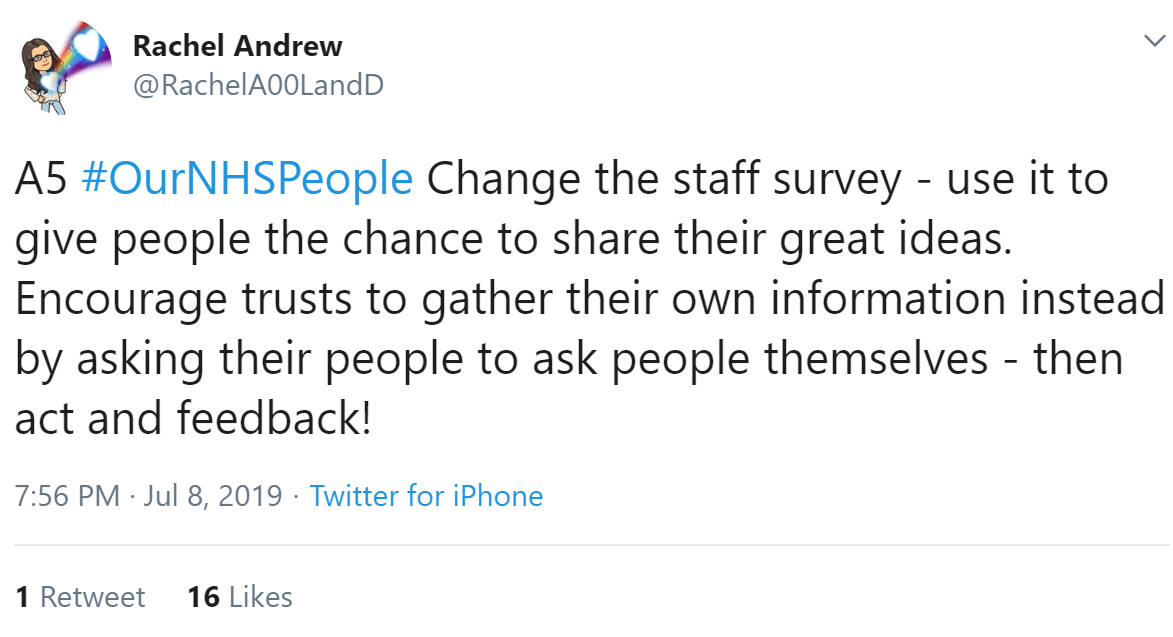
A5: Competence
Leadership with disciplined and inspiring values that pervade through an organisation, was an idea shared by Ian Daniels.
Invite the right people in to the room, giving resources to those most in need rather than the people who shout the most - as well as clarity, parity and leadership was asked for by Dr Cloutman-Green.
Ermintrude asked for the board to be genuinely accessible. There were diverse ideas around the topic of wellbeing. Many of the wellbeing ideas were simple, focused on ideas and behaviours.
Ananta Dave asked people to treat others how you would like to be treated.
Fairness and compassion for all was a contribution by Maria Zerega, and similarly Mubashshir Fazlee asked for value and respect. Jingy Alom asked for recognition, support, asking others if they are ok. Treating everyone fairly, and recognising that non-clinical are as important as clinical staff said Pink Lady April.


And as mistakes will happen, let's create a culture where we admit them, learn from them and create a climate where it's safe to try new innovations, and to fail observed Amy Beeton.
Ideas about personal, professional, and team development include Penny Fenton's idea for "skilled personal and professional development, supported by outstanding and creative supervision and support".
Help people find their strengths and provide lots of encouragement, suggested Ola Hill, and Maddie would like everyone to have opportunities to progress.
Bibi Matthews expanded on this, adding: "invest in making staff feel appreciated at work listen to them and get regular feedback from them clear development career pathway BAME staff treated with fairness and compassion and valued for their talent". More BAME people in senior roles was echoed by Melissa Therms.
 A similar suggestion was shared by Etain Clarke. Managers should spend at least one day a year in a clinical area, suggested Owen. Coffee roulette - (or randomised coffee trials as they can also be known) was offered by Cat.
A similar suggestion was shared by Etain Clarke. Managers should spend at least one day a year in a clinical area, suggested Owen. Coffee roulette - (or randomised coffee trials as they can also be known) was offered by Cat.Collaborative education opportunities was suggested by Kip Heath. More team days to build team cohesion was suggested by Kerry Taylor-John.

A5: Defining
Staff need to thrive, not just survive said Tina Hetherington. Finding a balance with workload and wellbeing to encourage more staff to step up - Pauline Smith observed that wearing long hours and insurmountable odds as a badge of honour discourages this. Madi Hoskin echoed this. Pace of work takes away from getting to know one another, and removes joy from work suggested Lisa Barrett. Em Wilkinson-Brice reflected that how we feel is just as important as what we do.
Solutions to these issues include ideas from Bridget Lees on mental health and self-care support for staff; and fast-track IAPT and physio for staff which happens at Worcestershire Health and Care NHS Trust. The importance of this was echoed by Prerana Issar.
Time is precious; an idea shared by Ermintrude was birthday leave; an extra day of annual leave, to be taken on individuals' birthdays, was given to staff as a reward for performing well at a previous organisation.

Improved IT was also shared by Victoria Annis, technology that works and is appropriate for the job from Anita Anderson. Claire Arditto said sorting things like IT out means staff can do their best work.
The end of the tweetchat

There were many positive tweets at the end. We also conducted a Twitter poll to evaluate reactions at the end of the tweetchat. These were the results:
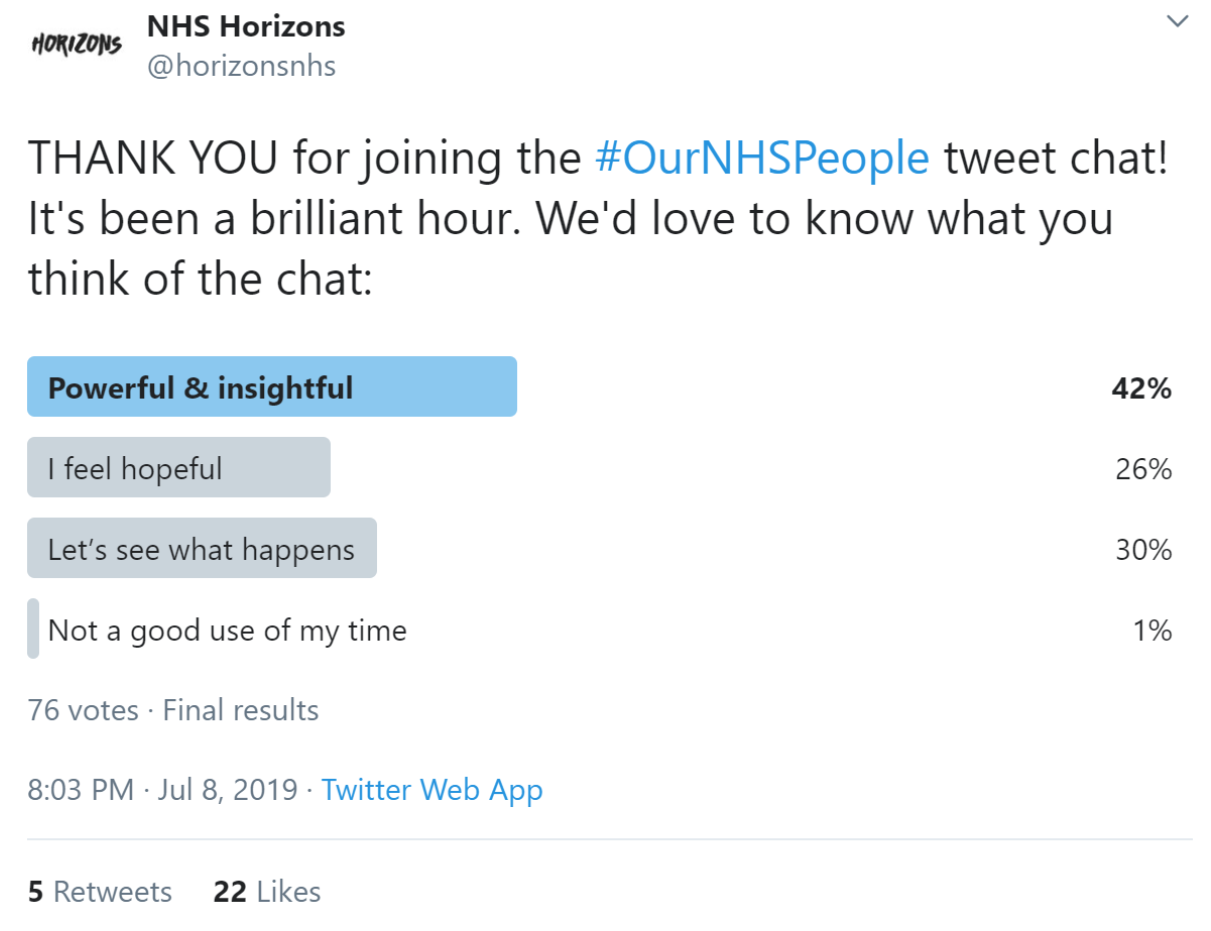
The poll results suggest that the tweetchat was a positive experience for most people. However, we can interpret the fact that the majority of people stated “I feel hopeful” or “let’s see what happens” as a message about the need for follow up. We can create a highly engaging tweetchat but will this be more than an hour of conversation? Will real change result?
Next steps
Two further tweet chats are planned by the best place to work workstream:
- August 12th 7pm: What can we do to improve how people in the NHS work in teams?
- September 9th 7pm: What do people who work in the NHS need from their leaders?
This first #OurNHSPeople tweetchat has shown how much energy and interest there is in helping to make the NHS the best place to work amongst hundreds of people who work for the NHS.
It demonstrates the potential not just for getting the views of people on making the NHS the best place to work but mobilising them to help make it happen. This tweetchat could be the start of a social movement.
Leigh Kendall and Helen Bevan, Horizons team
Appendix
Analysis of the tweets by themes
The Horizons team also reviewed the 5,581 tweets that were generated by the tweet chat in a bottom up way to identify specific themes. Overall, there was a lot of consistency in the content of the tweets. They fitted into a hierarchy of need:

Some tweets mentioned the need for more staff and how staff shortages create challenging work environments. However, the issues of flexible working, getting basic things right, being valued at work and a culture of compassion and kindness were far more prevalent in the tweetchat. In looking at the tweets as a whole, the positivity and hope within them shines through. Whilst they are realistic and represent a workforce under pressure, very few of the tweets make negative comments. These tweets give a sense of a workforce that has a lot of ideas and wants to help make the NHS the best place to work.
The top 10 key themes from the tweet chat:
- Our shared NHS purpose
- Flexible working practices
- Being valued
- Personal, professional and team development
- Leadership
- Getting basic things right for wellbeing
- Diversity and inclusion
- Innovation/ new ways of thinking and doing things
- Give power to NHS employees (build our agency)
- Recruitment and retention
Our shared NHS purpose
- Connecting our roles with NHS purpose
- Pride in being part of the NHS and supporting patients and families to be healthy
- Applying the values and (human rights) principles of the NHS to NHS employees
Flexible working practices
- The biggest theme of the tweetchat (these tweets were most likely to be retweeted).
- Flexibility in its widest sense, from flexible contracts to flexible training and career development, to flexible shift patterns to flexible working conditions to flexible venues for work
- Link between staff happiness, wellbeing and flexible working
“Personalisation”/personalised care for both patients and staff
Being valued
- Our staff as the biggest asset of the NHS
- Don’t take the goodwill of staff for granted
- All skills to be valued
- The human touch and being thanked/appreciated
- Small expressions of appreciation can make a big difference
- Celebrating success and celebrating excellence
Personal, professional and team development
- Supporting everyone to reach their potential
- More time for development
- More development opportunities
- More flexibility in how development happens
- More team development
Leadership
- Compassionate and kind leaders
- Leadership role modelling by senior leaders
- Creating shared purpose
- Boards with the courage to challenge national leaders
- Less hierarchy, more connected networks
- IT development and the balance between systems and people
- Seeing everyone as a leader, not just those with formal authority
- More support for mid-level managers and supervisors
- Giving people time, space and the support they need to care
Getting basic things right for wellbeing
- Being/feeling cared about as an individual
- Availability of healthy nutritious food
- Being able/encouraged to take proper breaks
- Having somewhere to eat
- Car parking (free)
- Rest facilities for night workers
- Less paperwork
- Proactive strategies to avoid burnout
- Knowing what is going on in my organisation
- IT systems that talk to each other
- Helping staff to stay healthy
Diversity and inclusion
- Valuing difference of all kinds
- Listening to voices that are different to the usual thinking
- Psychological safety for all
- Supporting staff from minority backgrounds (minority in a wide sense) to enter NHS careers and thrive in NHS careers
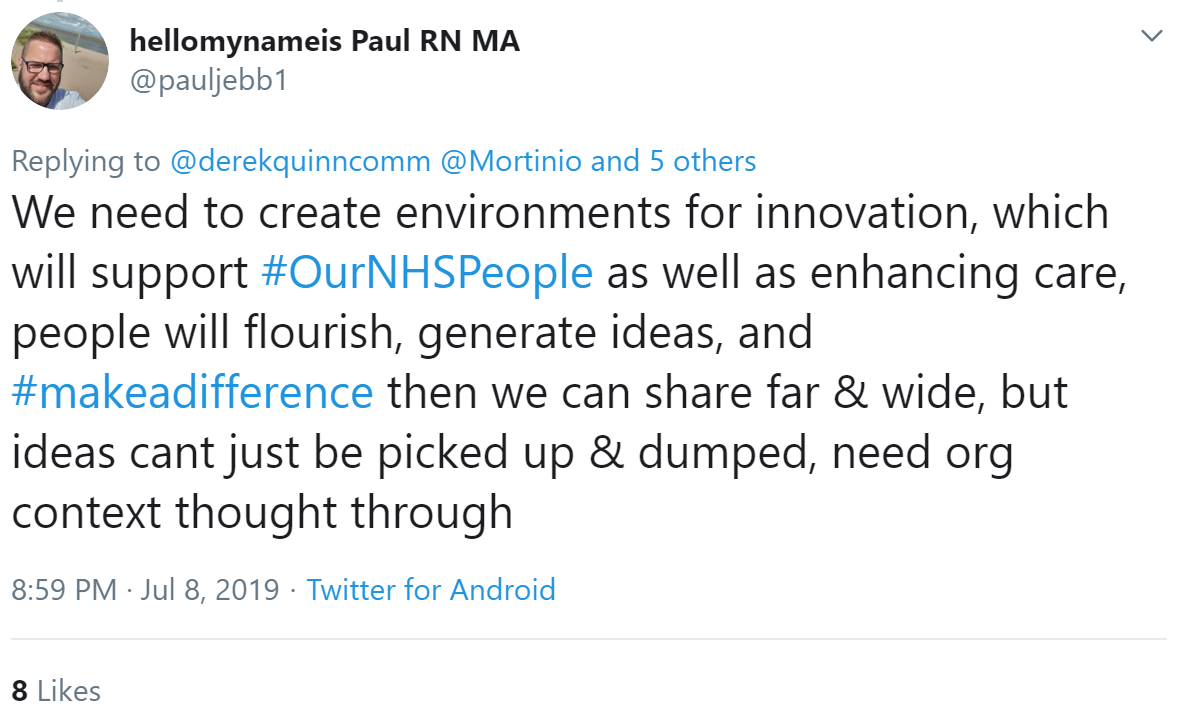
Innovation/new ways of thinking and doing things
- We cannot carry on as we are regarding NHS workforce: we need innovation at a massive scale
- Build space for innovation and a culture of innovation
- More systematic approaches for innovation
- Reward and celebrate innovation
- Safety 2 as well as Safety 1
- Hear more diverse voices
- Co-production with patients and families
- NHS staff are an army of innovators: let us help more with tacking the big challenges
Give power to NHS employees (build our agency)
- Give improvement skills to everyone who works in the NHS
- Give us time for improvement
- More systematic approaches to improvement; not a “nice to do” but a “must do” at every level of the NHS
- Give us new power
- “Break the rules”: we need to move beyond a permission culture
- Celebrate great outcomes
- Create ways where we can share our learning and good practice with others with similar interests
- Link to our intrinsic motivation (doing this because we want to) rather than making improvement part of a performance system
Recruitment and retention
- Shifting perceptions of potential recruits about what it means to work in the NHS (there is too much negativity about working in the NHS in the media)
- Meaningful, values-based recruitment
- Acting on employee feedback
- Need for campaigns focused on joy in work
- Exit interviews so we understand why people leave



/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-04-14-15-27-52-040-62583d78f636e9115805b2d5.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-08-05-09-59-36-465-62ecea08f636e906acfed639.jpg)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-28-14-57-17-405-62e2a3cdf636e9180c9835cb.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-20-10-16-56-533-62d7d618f636ea07987f6668.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-15-09-55-32-858-62d13994f636ea1398e71aa9.jpg)